What are the typical symptoms of allergic rhinitis?
Seasonal allergies (commonly referred to as Hay Fever) occur as a result of exposure to allergens at different times of the year. The most common presentation is allergic rhinitis (inflammation of the inner mucous membrane of the nose), with symptoms including itching, sneezing, rhinorrhea (runny nose), nasal congestion and itchy, watery eyes (allergic conjunctivitis). An individual may present with one or a variety of symptoms depending on the severity. Household allergens may also contribute to allergic rhinitis and typically occur year-round (termed perennial allergy).1
Could it be sinusitis (rhinosinusitis)? What makes it different from allergic rhinitis?
Rhinosinusitis or commonly referred to as “sinusitis” is defined as inflammation and/or mucosal thickening of 1 or more of the paranasal sinus cavities. It is classified as acute (occurring 4 weeks or less) that could be recurrent or chronic rhinosinusitis (lasting 12 weeks or more). As the paranasal sinus cavities are normally sterile, sinusitis usually occurs secondary to viral or bacterial respiratory infections. It is then possible that sinusitis may be mistaken for allergic rhinitis. The most common symptoms of sinusitis are characteristic of Upper Respiratory Tract Infection (URTI), including purulent nasal discharge and facial pain, headache, ear pain, fatigue and cough.
Treatment usually involves the use of analgesics/antipyretics and antibiotic therapy (if bacterial), and possibly decongestants.
When treating allergic rhinitis and symptoms don’t resolve with appropriate trial of medications (2-4 weeks), refer to a physician or a specialist for proper diagnosis.2,3,4
Are there any non-pharmacological treatments available?
Allergen avoidance is the first step in preventing symptoms but may not always be possible. Another non-pharmacological approach is the use of intranasal saline spray and irrigation which may provide some symptomatic relief through irrigation of allergen from the nasal mucosa. An allergy test (skin prick test) may help in identifying the allergen. Alternatively, an allergen-specific immunoglobulin (IgE) test, which requires a blood sample, is done when the skin test is inconclusive.5
What are some pharmacological options? 6, 7
When avoidance to environmental allergen is not possible, and nasal irrigation is not effective, there is a variety of pharmacotherapeutic options available:
- antihistamines
- decongestants
- corticosteroid nasal sprays
- allergen immunotherapy
Some of these medications are available in different preparations (oral, intranasal spray, eye drops) and are listed below.
Oral preparations – most oral preparations are available over-the-counter (OTC) and most provide the ease of use of once daily dosing. Loratadine and desloratadine are also available as syrups, while cetirizine is also available as a chewable tablet – an option for children. As they are ingested, there is a higher risk of systemic adverse effects than when given locally, but each individual will respond differently. The following are available as oral preparations:
- antihistamines: 1st and 2nd generation
- combination antihistamine/decongestants
- leukotriene receptor antagonist (LTRA)
Intranasal products – as applied locally, there is a lower risk of systemic adverse-effects when taken at usual dose (side-effects are localized). The onset of effect may also be faster than oral preparations:
- corticosteroids
- antihistamine
- anticholinergics
- decongestants
Combination Intranasal preparations – for treatment of resistant cases of allergic rhinitis (details below):
- corticosteroid/antihistamine
Ophthalmic preparations (eye drops) – topical treatment for ophthalmic symptoms as stand-alone therapy or adjunct (additional therapy):
- antihistamine/mast cell stabilizer
- mast cell stabilizers
When choosing the appropriate pharmacotherapy, numerous factors are considered, such as your allergy symptoms, severity, duration, your past response to medications, cost, as well as other medication and/or conditions you have. Have a conversation with your doctor or pharmacist to see which product is right for you. This article will focus on the most common treatments available. Table 1 describes the efficacy and indications of different treatment modalities for allergic rhinitis.
Table 1: Comparison of Symptom Relief in Allergic Rhinitis Therapies 7, 8, 9
|
Medication |
Rhinorrhea |
Congestion |
Sneezing |
Nasal Itch |
Eye Symptoms |
|
Oral antihistamines |
+ |
+/- |
+ |
+ |
+/- |
|
Decongestants |
– |
+ |
– |
– |
– |
|
Intranasal corticosteroids |
++ |
++ |
++ |
++ |
+/- |
|
Leukotriene receptor antagonists |
+ |
+ |
+/- |
+/- |
+/- |
|
Intranasal anticholinergics |
++ |
– |
– |
– |
– |
|
Intranasal antihistamines |
++ |
++ |
++ |
++ |
+/- |
Abbreviations:
– = no effect; +/- = modest or variable effect; + = moderately effective; ++ = effective
How to choose the right treatment for you
Treatment of mild and infrequent symptoms: 6, 7, 10
Typically, mild intermittent/infrequent symptoms are treated with oral antihistamines. They relieve most symptoms such as rhinorrhea, nasal itch, sneezing, and conjunctivitis, but may not be as effective for nasal congestion. Most of these medications are available over-the-counter (OTC), while some are available with a prescription. Most antihistamines are now available as “non-drowsy”, which are classified as 2nd generation antihistamines. The use of 1st-generation antihistamines (ex: diphenhydramine or Benadryl®; and chlorpheniramine or Chlor-Tripolon) for treatment of seasonal allergies is no longer recommended given their adverse effect profile as sedating and having anticholinergic side-effects ®. 10
Although not as common, certain individuals may still experience drowsiness with 2nd generation antihistamines, specially at higher doses. Among them, cetirizine, is more likely to cause sedation but not as much as 1st generation antihistamines. Newer antihistamines have come to market and are available by prescription only, but the data is still lacking, especially on their safety profile (Bilastine® and Rupall®).
Intranasal antihistamine levocabastine is also effective when used daily on an as-needed basis and provides the benefit of a more rapid onset with minimal systemic side-effects compared to oral antihistamines. Considering that cost may be a factor for certain individuals, oral preparation antihistamines are more readily available and less expensive than the nasal spray antihistamine.
As antihistamines are not effective for treatment of nasal congestion, decongestants can be added on an as-needed basis for breakthrough relief (discussed in the “Add-on” section below).
Antihistamine eye drops are also available. See “Adjunct treatments, specific symptoms and special population” section below.
Table 2: Common antihistamine preparations for treatment of mild and infrequent symptoms 6,7
|
2nd Generation antihistamines (oral):
Intranasal antihistamine:
Combination intranasal (antihistamine/corticosteroid):
|
|
Indications and duration:
|
|
Possible Side-effects:
|
|
Caution and Contraindications:
|
|
Additional Notes: 6, 11 Blexten®: newer prescription 2nd generation antihistamine for treatment of allergic rhinitis (patients ³ 12 y.o.). Also indicated for chronic spontaneous urticaria: pruritus (itching) and hives (³ 18 y.o.)
Rupall®: newer prescription 2nd generation antihistamine for treatment of allergic rhinitis (patients ³ 12 y.o.)
|
Treatment of moderate-severe rhinitis or persistent mild symptoms 6, 7
Intranasal corticosteroids are the 1st line treatment for moderate to severe allergic rhinitis. When compared to antihistamines and leukotriene antagonists, they are shown to be more effective in relieving symptoms, especially in relieving nasal congestion and ocular symptoms associated with allergic rhinitis. The onset of effect is within 6-8 hours of 1st dose but full effect could be experienced up to 2 weeks. Regular use of intranasal corticosteroid is more effective than intermittent use. 12
The combination antihistamine/corticosteroid, azelastine/fluticasone (Dymista®) is a viable option for persistent symptoms or in severe allergic rhinitis by taking advantage of the combination of two different mechanism of actions of the two medications. 13
As administered locally, systemic effects are less likely but local irritation of the nasal mucosa is common (dryness and nosebleed). To minimize the local side-effect with intranasal corticosteroids and with other intranasal products, they should be sprayed towards the turbinate (away from the nasal bridge, pointing upwards and aimed laterally toward the tip of the ear). The corticosteroid preparations have different systemic bioavailability (how much is transferred systemically from the local site) which translate to systemic adverse-effects (eg. Hypothalamix Pituitary Adrenal axis and small significant effect on child’s growth) – a factor that is considered when choosing the right intranasal medication. The table below describes their bioavailability and their effect. 14, 15
Table 3: Intranasal corticosteroid for treatment of moderate to severe rhinitis 6, 7
|
Intranasal corticosteroids (INCS):
Combination product (antihistamine/corticosteroid):
|
|||||||
|
Indications and duration:
|
|||||||
|
Possible Side-effects:
|
|||||||
|
Additional Notes:
|
Add-on Therapy 6, 7
Decongestants (available as oral or intranasal spray, as stand-alone product or combination) can also be also be added to antihistamines to relieve nasal congestion for a short period of time (breakthrough). Additionally, intranasal decongestants can used as an adjunct to intranasal corticosteroid to improve its efficacy, especially at the onset of symptoms. Additionally, inhaled decongestants appear to have a stronger effect on nasal obstruction than oral decongestants. 16, 17
Given their pharmacological properties, the risk of systemic adverse-effects should be considered, especially with oral preparations (see below). The oral form is likely to cause more systemic effects than the topical intranasal preparation. That said, topical/intranasal preparations have a potential to cause rhinitis medicamentosa (rebound congestion). As such, their use should be limited to 3-7 days. 6, 7
Table 4. Decongestants as adjunct and breakthrough therapy
|
Add-On Decongestants Oral form in combination with 2nd Generation Antihistamines preferred
Intranasal spray
|
|
Indications and properties:
Onset: Within the day Monitor: Improvement in congestion within the day up to 3-4 days |
|
Common Possible Side-effects:
|
|
Caution and Contraindications:
|
Adjunct treatments, specific symptoms and special population:
A person experiencing allergic rhinitis may present with some or all of the symptoms described above. Additionally, some patients may be contraindicated on certain medications. The following summarizes options available for these specific conditions.
Rhinorrhea (runny nose)18
Intranasal anticholinergic ipratropium (generics) is indicated when rhinorrhea is the only symptom present. It is a viable option for sneezing caused by the runny nose, and especially helpful with “skier’s nose”.
Ocular symptoms and ophthalmic preparations 6, 7, 19
Ophthalmic preparations are indicated for treatment of ocular symptoms (conjunctivitis due to allergies – itchy, gritty, watery eyes), when either allergic conjunctivitis is the only set of symptoms present, or as an adjunct therapy when oral antihistamine, INCS and leukotriene receptor antagonists are ineffective in providing relief.
Two types of eye drops are available. Their different characteristics as described below are factors to be considered in deciding the appropriate treatment.
Antihistamines and Mast Cell Stabilizers (Dual effect):
- ketotifen (Zaditor ®, generics – by prescription only)
- olopatadine (Pataday®, Patanol®, generics – by prescription only)
Onset: symptomatic relief in minutes, with lasting effect up to 12 hours
Other considerations:
- Pataday® is available as once daily dosing, applied as 1 drop to affected eyes
- Patanol® is available as twice daily dosing, applied as 1-2 drops to affected eyes
- Available by prescription and therefore more expensive, but with more rapid effect than the products below
Mast Cell Stabilizers:
- sodium cromogylate (Opticrom, generics – OTC)
- nedocromil (Alomide® – by prescription)
- lodoxamide (Alocril – by prescription)
Onset: longer onset of symptomatic relief (a few days up to 4 weeks)
Other considerations:
- Frequent administration (four times daily) initially may be required for optimal benefit
- Opticrom® or its generics is a less expensive option that’s available over-the-counter
Special Population 6, 7, 16
Pregnancy/breastfeeding
In general, topical preparations (intranasal and ophthalmic) are preferred in pregnancy and breastfeeding as side-effects are mostly localized. Inhaled corticosteroids are favoured as 1st-line therapy during pregnancy given the minimal side-effects and its efficacy for treatment of allergic rhinitis compared to antithistamines (oral and topical). Inhaled decongestants and saline nasal spray are also viable options. Avoid use of oral decongestants during 1st trimester due to possible malformations. 2nd generation antihistamines are preferred due to lower risk of decreased milk production in the breastfeeding mother and infant somnolence.
Elderly and patients with comorbid conditions
The elderly population is more likely to have other medical conditions and are therefore more susceptible to adverse-effects. Considering their sensitivity to these medications, topical preparations are the preferred choice of treatment. As described above, individuals with hypertension or other cardiac conditions, closed-angle glaucoma, enlarged prostate, hyperthyroidism should take extra precaution when taking products with decongestants, more importantly with oral preparations. Avoid decongestants when these conditions are uncontrolled.
Summary
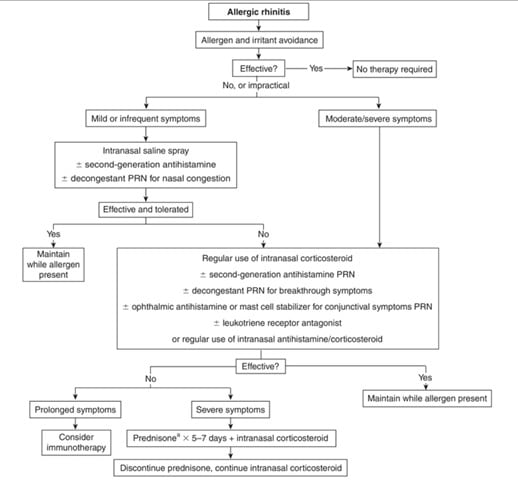
A treatment algorithm for allergic rhinitis is provided below on Figure 1. Note that mild or infrequent is defined as symptoms lasting <4 days per week or <4 weeks. Persistent symptoms are defined as lasting more than 1-2 months and are considered moderate. The number of symptoms experienced and the effect on a patient’s quality of life is also factored in choosing the appropriate therapy.6,7
Figure 1. Treatment algorithm for Allergic Rhinitis 6

Sources:
- Rhinitis – Ear, Nose, And Throat Disorders – MSD Manual Consumer Version”. 2019. MSD Manual Consumer Version. Accessed September 8 2019. https://www.merckmanuals.com/en-ca/home/ear,-nose,-and-throat-disorders/nose-and-sinus-disorders/rhinitis#v28482714.
- Desrosiers M, Frenkiel S, Hamid QA et al. Acute bacterial sinusitis in adults: management in the primary care setting. J Otolaryngol 2002;31(Suppl 2):2S2-14.
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg 2015;152(2 Suppl):S1-S39.
- Fryters S, Blondel-Hill E. Acute Rhinosinusitis. In: CTC [Internet]. Ottawa (ON): Canadian Pharmacists Association; c2019 [updated MAY 2018; cited 2019 Sept 06]. Available from: http://www.myrxtx.ca. Also available in paper copy from the publisher.
- Allergic Rhinitis – Immunology; Allergic Disorders – MSD Manual Professional Edition”. 2019. MSD Manual Professional Edition. Accessed September 8 2019. https://www.merckmanuals.com/en-ca/professional/immunology-allergic-disorders/allergic,-autoimmune,-and-other-hypersensitivity-disorders/allergic-rhinitis.
- Keith P. Allergic Rhinitis. In: CTC [Internet]. Ottawa (ON): Canadian Pharmacists Association; c2019 [updated AUG 2019; cited 2019 Sept 06]. Available from: http://www.myrxtx.ca. Also available in paper copy from the publisher.
- Kendrick J. Allergic Rhinitis. In: CTMA [Internet]. Ottawa (ON): Canadian Pharmacists Association; c2019 [updated AUG 2018; cited 2019 Sept 06]. Available from: http://www.myrxtx.ca. Also available in paper copy from the publisher.
- Wilson AM, O’Byrne PM, Parameswaran K. Leukotriene receptor antagonists for allergic rhinitis: a systematic review and meta-analysis. Am J Med2004;116:338-4.
- Scadding GK, Durham SR, Mirakian R et al. BSACI guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy 2008;38:19-42.
- Wallace DV, Dykewicz MS, Bernstein DI et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol2008;122:S1-84.
- CPS [Internet]. Ottawa (ON): Canadian Pharmacists Association; c2019 [updated 2018 DEC 13; cited 2019 SEP 06]. Blexten [product monograph]. Available from: http://www.e-cps.caor http://www.myrxtx.ca. Also available in paper copy from the publisher.
- Laekeman G, Simoens S, Buffels J et al. Continuous versus on-demand pharmacotherapy of allergic rhinitis: evidence and practice. Respir Med2010;104:615-25.
- Carr W, Bernstein J, Lieberman P et al. A novel intranasal therapy of azelastine with fluticasone for the treatment of allergic rhinitis. J Allergy Clin Immunol 2012;129(5):1282-9.
- Bielory L, Chun Y, Bielory BP et al. Impact of mometasone furoate nasal spray on individual ocular symptoms of allergic rhinitis: a meta-analysis. Allergy2011;66(5):686-93.
- Dykewicz MS, Wallace DV, Baroody F et al. Treatment of seasonal allergic rhinitis: an evidence-based focused 2017 guideline update. Ann Allergy Asthma Immunol2017;119:489-511.
- Wallace DV, Dykewicz MS, Bernstein DI et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol2008;122:S1-84.
- Plaut M, Valentine MD. Clinical practice. Allergic rhinitis. N Engl J Med2005;353:1934-44.
- Grossman J, Banov C, Boggs P et al. Use of ipratropium bromide nasal spray in chronic treatment of nonallergic perennial rhinitis, alone and in combination with other perennial rhinitis medications. J Allergy Clin Immunol1995;95(5 Pt 2):1123-7.
- Castillo M, Scott NW, Mustafa MZ et al. Topical antihistamines and mast cell stabilisers for treating seasonal and perennial allergic conjunctivitis. Cochrane Database Syst Rev2015;(6):CD009566.

