How to Avoid and Treat Travellers’ Diarrhea
What is Travellers’ Diarrhea (TD)
- TD is defined as having 3 or more unformed stools within a 24 hour period associated with one of the following: Nausea, vomiting, abdominal pains, cramps, fever, and in severe cases bloody stools.
- Usually occurs within first week of arriving at destination
- Self limiting and resolves within two days for 50% of travellers, no more than a week
- NOT life threatening in most cases
Causes of TD
Organisms that can cause TD:
- Bacteria: Enterotoxigenic Escherichia coli, Enteroaggregative Escherichia coli, Campylobacter, Salmonella, Shigella species as well
- Viruses: Norovirus, Rotavirus
- Protozoa: Giardia, Crytosporidium
Other notes:
- TD is due to poor hygiene
- Bacteria spread through food, unsanitary drinking water, or the conditions in which the food was prepared
- More likely to happen in third world countries than developed countries
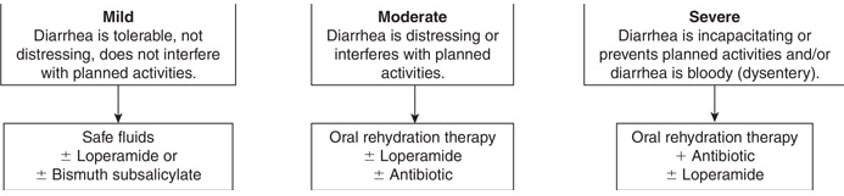
Classifying TD
- Mild: Diarrhea is tolerable and does not interfere with planned activities
- Moderate: Diarrhea is distressing and interferes with planned activities
- Severe: Diarrhea prevents planned activities and consists of bloody stools
- Persistent: More than two weeks
Preventing TD – Nonpharmacological
- Drink only boiled or bottled water; can use chlorine or iodine drops in clear water
- Avoid ice cubes
- Eat fruits and that have only been peeled
- Avoid salads and raw vegetables
- Avoid food from street vendors
- Eat meats that have only been cooked thoroughly and well done (no medium rare, rare etc…)
- Wash hands with soap and water, hand sanitizers
- Boil it, Cook it, Peel it or forget it!
Preventing TD – Pharmacological
Avoid use of proton pump inhibitors and H2 receptor antagonists while travelling: Decreased stomach acidity increase risk of TD
Vaccines:
- Dukorol Vaccine – protects against Enterotoxigenic Escherichia coli: for anyone 2 years and older; 1st dose 2-6 weeks before departure, 2nd dose 1 week before departure, both on empty stomach; most effective for Latin America, Africa, South Asia, Southeast Asia.
Non-antibiotics:
- Bismuth Subalicylate: 524 mg (2 tablets) four times a day; do not use for more than 3 weeks, or < 3y/o; 50% effective; blackened tongue and stools is a side effect.
- Probiotics: Lactobacillus GG (Culturelle) and Saccharomyces boulardii (Floraster) have been studied in prevent TD. Also, HMF Travel probiotics by Genestra combines five probiotic strains from Lactobacillus, Bifidobacterium and Saccharomyces genera to promote a healthy gut flora and support gastrointestinal health. A number of travel-related factors, including unfamiliar food or water, stress and jet-lag, can all affect the normal composition of gut bacteria.
*Notes about HMF Travel Probiotic:
- These probiotics are also dairy and gluten free and are also vegan capsules
- HMF Travel Probiotics consist of the following key probiotics: Saccharomyces boulardii: A study showing travelers taking 250 mg (5×109 CFU) and 500 mg (10×109 CFU) starting 5 days before their trip and throughout the duration of their trip resulted in less gastrointestinal discomfort and diarrhea during their travel when compared to palcebo3 The travelers were travelling to Africa and Southeast Asia; Lactobacillus acidophilus and Bifidobacterium bifidum: these are two natural gut probiotics, a study involving travellers to Egypt had the probiotics listed above given three times a day at 3 x 109 CFU per dose for the duration of their trip. This resulted in less gastrointestinal discomfort and diarrhea when compared to placebo.
- A placebo controlled trial shows that the results here are more effective than not taking anything in order to prevent travelers diarrhea when traveling. It is important to note that the results were obtained from self questionnaires given to the travelers.
Antibiotics:
- Reduce the risk of TD by 90%
- Prophylactic use of antibiotics is no longer recommended unless the patient is immunocomprimised
- Their use should be limited to three weeks
- Antibiotics may lead to resistance and may even cause diarrhea
- Fluoroquinolones are used as prophylaxis in adults and non pregnant females. Ciprofloxacin 500 mg once daily; Levofloxacin 500 mg once daily; or Norfloxacin 400 once daily
-
Treating TD – Nonpharmacological
Staying hydrated:
- Drinking lots of water
- Avoid fatty and oily foods
- Avoid natural laxatives (eg. Coffee, alcohol, excessive amounts of fruits and veggies)
- Avoid fibers that are hard for the stomach to break down, this may lead to bloating
Oral Rehydration Therapy:
- ½ teaspoon of salt and 6 teaspoons of sugar in 1 L of water – max 2L per day
Treating TD – Pharmacological
Oral Rehydration Therapy:
- Pedialyte or Gastrolyte
Bismuth Subsalicylate:
- Decreases frequency and duration of diarrhea
- 524 mg every hour as needed (Max 4.2 grams per day)
Loperamide:
- Relieves mild to moderate diarrhea by working as an antimotility agent
- Should NOT be used if one has a fever and or bloody stools
- Do not use in < 2y/o and for more than 2 days
- 4 mg initially then 2 mg after each lose stool (Max 16 mg/day)
Antibiotics:
- Fluoroquinolones: Ciprofloxacin 500 mg BID x 3 days OR 1000 mg x 1 dose; Levofloxacin 500 mg daily for 3 days OR 1000 mg x 1 dose; Norfloxacin 400 mg BID x 3 days OR 800 mg x 1 dose. NOT recommended in Southeast Asia or the Indian Subcontinent. Avoid if pregnant
- Macrolides: Azithromycin 500 mg once daily x 3 days OR 1000 mg x 1 dose. Children dosing: 10 mg/kg (Max 500 mg) x 3 days
-
When you should use your Antibiotics?
Antibiotics should only be used when the diarrhea is very severe, if there is blood present in the stool or if the traveller has a fever present. Once used, the diarrhea should decrease or be completely gone within 48 hours of starting the antibiotic.
How should a traveller carry a self assessment?
Summary
- Hygiene is KEY
- Boil it, cook it, peel it, or forget it
- Stay hydrated
- Loperamide should NOT be used in bloody stools
- Use antibiotics for treatment when diarrhea is severe, a fever is present or stools are bloody
- Antibiotics are not recommended as prophylaxis
- Diarrhea persistent for two weeks, or 48 hours after starting an antibiotic should seek medical attention
- ALWAYS purchase medications and ORT before travelling
References
1. Green Laurence & Libman Michael. (2017). Travellers Diarrhea. Compendium of Therapeutics. Cited on January 16 2020.
2. Connor BA. Travelers’ diarrhea. In: Centers for Disease Control and Prevention and Brunette GW, editors. CDC Health information for international travel. Oxford University Press, 2014. Available from: http://wwwnc.cdc.gov/travel/yellowbook/2014/chapter-2-the- pre-travel-consultation/travelers-diarrhea
3. McFarland Lynne (2007). Meta-analysis of Probiotics for the Prevention of Traveler’s Diarrhea. Travel Medication and Infectious Disease 5(2). 97-105. DOI: 10.1016/j.tmaid.2005.10.003
4. Black F.T et al.(1989) Prophylactic Efficacy of Lactobacilli on Travelers Diarrhea. Travel Medicine. 333 -335. DOI: 10.1007/978-3-642-737772-5_70
