Testosterone Replacement Therapy
Testosterone Replacement Therapy is prescribed when lab results indicate that a patient’s testosterone is too low. In many cases, low testosterone may be causing a lower sex drive. In other cases, low testosterone can cause a whole host of other issues including lack of energy, general fatigue, loss of memory, and sharpness. All of these symptoms are generally referred to as “Andropause”. Increasing testosterone levels can help with all of these issues and studies have shown that it can also protect from heart disease and stroke. Testosterone can be replaced with pills, patches, injections, and lotions. Many years ago, there was a myth perpetuated that testosterone replacement therapy led to prostate cancer. Repeated studies have shown that it does not contribute to prostate cancer and in fact, replacement of testosterone in deficient patients can actually have enormous beneficial overall health effects and protect against heart disease and stroke.
What is the definition of testosterone deficiency (TD)?
TD is a clinical and biochemical syndrome that may occur in men in association with advancing age; however, younger men with certain conditions may also be affected. The condition is characterized by deficient testicular production of testosterone, with or without changes in receptor sensitivity to androgens. It may affect multiple organ systems and can result in significant health consequences and a negative impact on quality of life.
What is the prevalence of testosterone deficiency (TD) among Canadian men?
The prevalence of TD varies between populations and is difficult to determine in the absence of widespread, routine testing, which is currently not the standard of care. Current studies evaluating the true prevalence of TD are conflicting due to variable reporting measures, testosterone level cut-offs, and testing protocols. The crude Canadian prevalence of biochemical TD is estimated to be approximately 25% among men aged 40–62 years. The rate of TD increases with age. Appreciating that prevalence rates will vary based on case definitions and biochemical testosterone thresholds, the prevalence of TD is estimated to be 4–12% in men aged 50–59 years, 9–23% in men aged 60–69 years, and 28–49% in men over 70 years old.
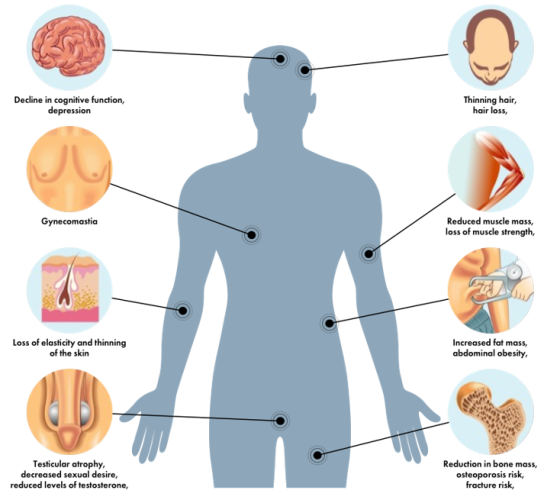
What are the common signs and symptoms of testosterone deficiency (TD)?
TD may present with a variety of clinical manifestations, including sexual, cognitive, and physical/structural signs and symptoms. Common signs of TD include decreased libido and vitality, sexual dysfunction, fatigue, and/or mood changes. The signs and symptoms of TD are not exclusive to this syndrome and are commonly associated with other conditions related to male aging. As such, the clinical presentation should be correlated with biochemical confirmation of low/equivocal serum testosterone levels.
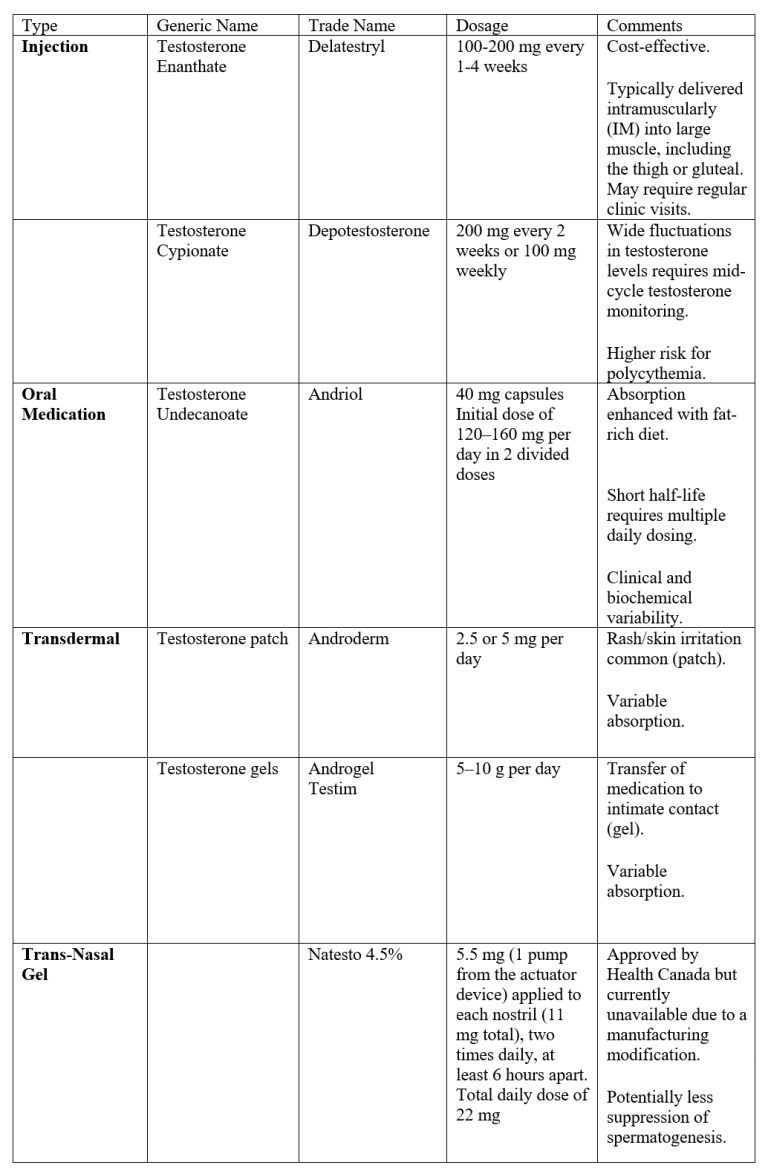
Treatments for testosterone deficiency (TD)
Estrogen Replacement Therapy
Menopause is the natural point in a woman’s life when her ovaries stop producing the hormones estrogen and progesterone and her menstrual periods stop. This usually happens between the ages of 45 and 55 but can vary. A woman may reach menopause early as a side effect of medical treatment such as chemotherapy or having her ovaries removed.
Hormone therapy (HT) is one of the government-approved treatments for relief of menopausal symptoms. These symptoms, caused by lower levels of estrogen at menopause, include hot flashes, sleep disturbances, and vaginal dryness. HT is also approved for the prevention of osteoporosis.
There are three benchmark stages of natural menopause:
– Perimenopause (or the menopause transition) is the span of time between the start of symptoms (such as erratic periods) and 1 year after
the final menstrual period.
– Menopause is confirmed 1 year (12 months) after the final menstrual period.
– Postmenopause is all the years beyond menopause.
Hormone Therapy (HT)
There are two basic types of HT:
1. ET means estrogen-only therapy. Estrogen is the hormone that provides the most menopausal symptom relief. ET is prescribed for women
without a uterus due to a hysterectomy.
2. EPT means combined estrogen plus progestogen therapy. Progestogen is added to ET to protect women with a uterus against uterine
(endometrial) cancer from estrogen alone.
There are two general ways to take HT:
1. Systemic products circulate throughout the bloodstream and to all parts of the body. They are available as an oral tablet, patch, gel,
emulsion, spray, or injection and can be used for hot flashes and night sweats, vaginal symptoms, and osteoporosis.
2. Local (non-systemic) products affect only a specific or localized area of the body. They are available as a cream, ring, or tablet and can be
used for vaginal symptoms.
What are the benefits of HRT?
Combined HRT may help relieve menopausal symptoms, protect against osteoporosis (thinning of the bones) and reduce the risk of colon cancer.
What are the risks of HRT?
Research shows that long-term use of combined HRT (for 5 or more years) increases the risk of breast and ovarian cancer, heart disease, stroke and pulmonary embolism (blood clots in the lungs). The research suggests that the risks of long-term combined HRT use outweigh the benefits for most women.
The decision to take HRT is personal and should be made with the help of your doctor. Concerns about cancer, heart disease and stroke should be discussed when considering the benefits and risks of HRT.
Alternatives to HRT
If you are experiencing any of the following:
Hot flashes
– Get as much exercise as you can.
– Choose light clothing and wear it in layers that can be removed.
Vaginal dryness
– Use a water-soluble lubricant or moisturizer available at your pharmacy.
– Ask your doctor about a vitamin E vaginal suppository or cream to help relieve symptoms.
Trouble sleeping
– Being active lowers stress and improves your overall well-being, which may help you sleep better.
– Try relaxation techniques. Deep breathing, massage or yoga may help reduce your stress levels.
– Sip chamomile tea or tea with valerian root at bedtime. Avoid caffeine and alcohol, they can make menopausal symptoms worse.
Bioidentical Hormones
Bioidentical hormones are made in a lab. They are based on compounds found in plants. They have the same structure as the hormones your body makes. Many commonly prescribed forms of estrogen and progesterone are bioidenticals. Some examples include: Estrace and Prometrium. These types are approved and regulated by Health Canada, and they are made by drug companies. Some bioidentical hormones are available in a compounding pharmacy. Compounded bioidentical hormones may be put into a capsule, a skin cream or gel, a tablet to dissolve under your tongue, a suppository, or a nose spray.
The interest in a more natural approach to hormone therapy has focused attention on bioidentical hormones. They’re not found in this form in nature but are made, or synthesized, from a plan chemical extracted from yams and soy.
Bioidentical estrogens are 17 beta-estradiol, estrone, and estriol. (Estradiol is the form of estrogen that deceases in menopause).
Bioidentical progesterone is simply progesterone. It’s micronized (finely ground) in the laboratory for better absorption in the body.
Commercially available bioidentical estradiol comes in several forms, including pill, patch, cream and various vaginal preparations. Micronized progesterone comes in a capsule or as a vaginal gel. See chart below.
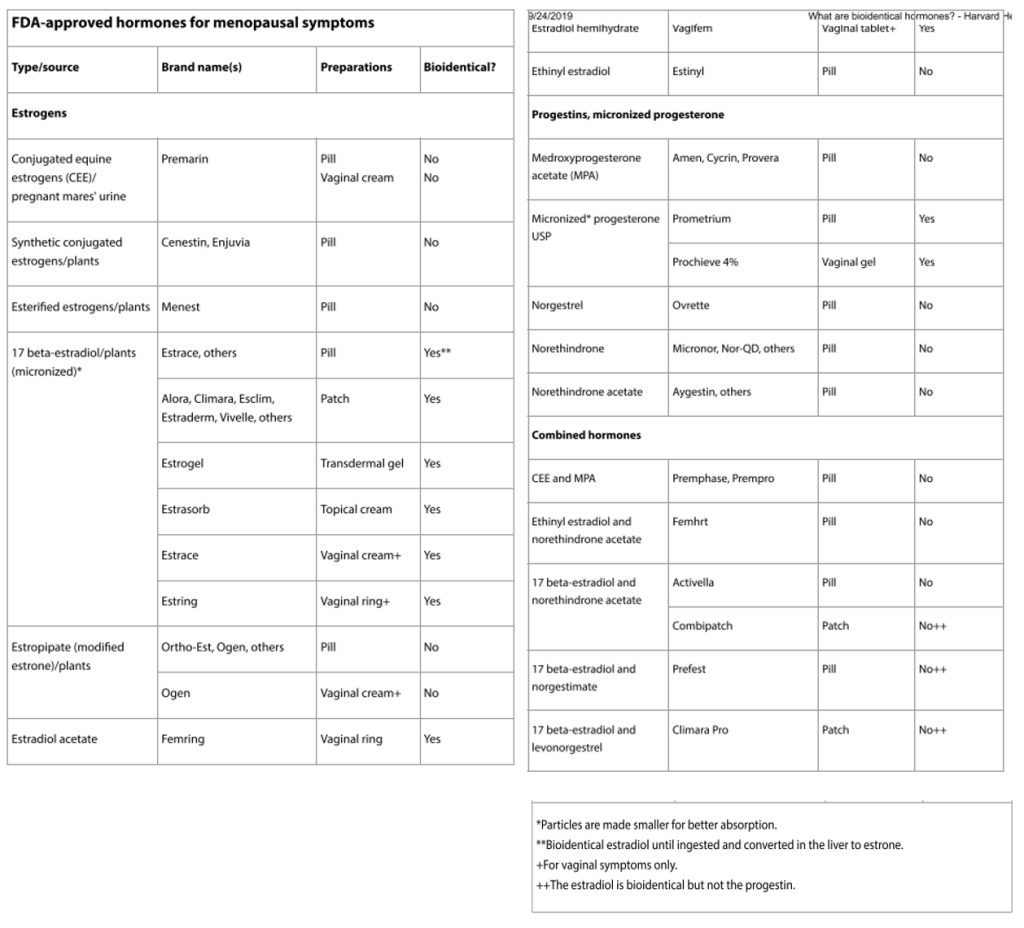
Compounded Hormone Replacement Therapy
One size doesn’t fit all. Compounded hormones can help individualize treatment. Custom compounding is necessary only when a clinician wants to prescribe hormones in combinations, doses, or preparations (such as lozenges or suppositories) not routinely available, or to order hormones not approved for women, such as testosterone and DHEA. Compounding pharmacies use some of the same ingredients that are made into FDA-approved products.
Example: Bi-est is commonly prescribed in estrogen replacement and is a combination of estradiol (E2) and estriol (E3). Traditionally the prescription is written as 80% E3 and 20% E2. The compound prescription should be guided by the results of the patient saliva tests* and can be any percentage of E2/E3 that is suitable for the patient. Compounded estrogen for hormone replacement always needs to be prescribed transdermally or transvaginally.
*The salivary 28-day hormone test is a comprehensive assessment of (E2) estradiol, (P4) progesterone, and testosterone over a 28-day period of a female’s regular menstrual cycle.
Traditionally, compounding is used to provide treatment for patients when the exact products needed are not commercially available or when different ingredients, preservatives, or routes of administration are required because of patient intolerances (eg, allergy) or needs (eg, inability to swallow an oral pill). For example, there is an FDA-approved progesterone product that contains peanut oil. A prescription to compound progesterone to eliminate the peanut oil can allow a patient with a peanut allergy to use the drug safely. Additionally, cost and access concerns may prompt consideration of compounded vaginal formulations of estrogen or progesterone, for which the quality control regarding potency and vehicle (cream or ointment) should be discussed with the compounding pharmacy. Far removed from the traditional uses of compounding is the practice of blending commercially available drug products in proportions tailored to an individual patient. Many compounded bioidentical menopausal hormone therapy preparations fall into this category.
Natural Products for Menopause
Herbal remedies that are sometimes taken for menopause symptoms include:
Evening primrose oil
The seeds of evening primrose (Oenothera biennis) are used to make evening primrose oil. This flowering plant is native to central and eastern North America, and its seed oil is frequently used to treat menopause symptoms like hot flashes and bone loss.
Black cohosh
Black cohosh (Actaea racemosa) is a flowering plant native to the eastern regions of North America. Long used in Native American herbal medicine to treat a variety of illnesses, it’s currently most often taken to alleviate night sweats and hot flashes associated with menopause.
Ginseng
Ginseng is one of the most popular herbal medicines worldwide. Used for centuries in traditional Chinese medicine, it’s said to boost immune system, heart health, and energy levels. Several types exist, but Korean red ginseng is most frequently studied in relation to menopause. It may bolster sex drive and improve mood and general sense of well-being in menopausal women.
St John’s wort
St. John’s wort is a well-known treatment for mild depression. But it might also have a special benefit for women during menopause. There’s some evidence, particularly when combined with black cohosh, that St. John’s wort can improve mood and smooth the mood swings tied to menopause.
Red clover
Red clover (Trifolium pratense) is an herbaceous flowering plant in the legume family. It’s a rich source of isoflavones. These compounds function similarly to the hormone estrogen and may help alleviate symptoms associated with the decline in estrogen production that occurs with menopause. Red clover is frequently used to treat or prevent various menopause symptoms, including hot flashes, night sweats, and bone loss.
