Lupron Depot Injections for Endometriosis Use
Taking Lupron Depot Alone:
Lupron Depot® (leuprolide acetate for depot suspension) 3.75 mg or 11.25 mg is used for the management of endometriosis, including pain relief and reduction of endometriotic lesions.
Taking Lupron Depot in Combination with Norethindrone Acetate:
Lupron Depot 3.75 mg or 11.25 mg in combination with norethindrone acetate is used for initial management of the painful symptoms of endometriosis and for management of recurrence of symptoms.
Use of norethindrone acetate in combination with Lupron Depot 3.75 mg or 11.25 mg is referred to as add-back therapy, and is intended to reduce the thinning of bone and reduce hot flashes associated with use of Lupron Dept 3.75 mg or 11.25 mg.
Limitations of Use:
The total duration of therapy with Lupron Depot 3.75 mg or 11.25 mg plus add-back therapy should not exceed 12 months due to concerns of bone thinning.
Endometriosis
Endometriosis is one of the most common gynecological disorders, affecting approximately 10% of all women in their childbearing years.
It’s not clear why endometriosis occurs, but we can help you understand what happens in your body. Endometriosis occurs when the endometrial lining normally found inside the uterus begins to grow outside the uterus. These growths are called lesions. They may grow on the ovaries, fallopian tubes, or other areas near the uterus. The lesions can bleed and break down each cycle, causing scar tissue and adhesions (scarring that binds tissues together).
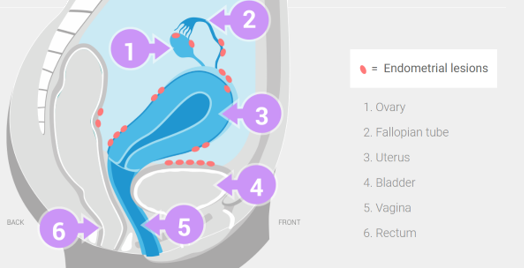
Endometrial tissue builds up in the uterus every cycle, but when it grows outside the uterus, it can cause painful symptoms.
Hormones, such as estrogen, can stimulate the growth of endometriosis. When endometrial tissue grows outside the uterus, it reacts to cyclic changes in hormones, but doesn’t necessarily respond the same way normal endometrial tissue inside the uterus does. Unlike the lining inside the uterus that sheds and leaves the body with each menstrual period, endometrial tissue can grow, bleed, and possibly form scar tissue on areas outside the uterus.
These events can cause painful endometriosis symptoms, such as:
– Recurring pelvic pain
– Painful intercourse
– Painful and/or heavy periods
Many women with endometriosis have no symptoms.
What is Lupron Depot?
Lupron Depot is a prescription medication for the management of endometriosis, given as an injection by a healthcare professional. It can help relieve the pain of endometriosis and reduce endometriotic lesions. Lupron Depot has been prescribed by doctors since 1990.
Lupron Depot offers 2 different dosing options for treatment, both of which can be combined with Add-back therapy from day 1 in appropriate patients:
– Injected once every 3 months (11.25 mg dose)
– Injected once each month (3.75 mg dose)
How does Lupron Depot work?
Lupron Depot suppresses the hormones that cause endometrial tissue to grow. Lupron Depot therapy suppresses the signals from the pituitary gland in the brain to the ovaries, which stimulate estrogen production. By doing this, Lupron Depot injections also suppress the hormones that cause endometriosis to grow.
Suppressing the hormones helps:
– Provide endometriosis pain relief
– Reduce endometriotic lesions
Lupron Depot Reduces Endometriosis Pain
By suppressing the hormones that feed endometriosis, Lupron Depot injections can help reduce your endometriosis pain and reduce the size of endometriotic lesions. In 2 studies of women undergoing endometriosis treatment with Lupron Depot 3.75 mg for 6 months, 96% of women had relief from painful periods after their initial 6 months of therapy. Many also experienced relief from painful intercourse, pelvic tenderness, and pelvic pain.
Common Side Effects
In clinical trials, the most common side effects of Lupron Depot, occurring in >10% of patients, include hot flashes/sweats, headache/migraine, decreased libido, depression/emotional lability, dizziness, nausea/vomiting, pain, vaginitis, and weight gain.
Add-back Therapy and Side Effects
When Lupron Depot is used alone, bone thinning and hot flashes can occur. Along with Lupron Depot injections, your doctor may prescribe Add-back therapy. Add-back is a daily pill that you take while on Lupron Depot therapy to add back a small amount of the hormone progestin, which can help you manage certain side effects, without interfering with the way Lupron Depot works.
Who Should Not Take Lupron Depot?
You should not receive Lupron Depot if you:
– Are or may become pregnant
– Have undiagnosed vaginal bleeding
– Have experienced any type of allergic reaction to Lupron Depot, or similar drugs
– Also do not take Lupron Depot 3.75 mg if you are breastfeeding
You should not receive Add-back plus Lupron Depot if you have or have had any of the following conditions:
– Clotting disorder
– Stroke
– Impaired liver function or liver disease
– Breast cancer
Lupron Depot Injections for Uterine Fibroids
Lupron Depot® (leuprolide acetate for depot suspension) 3.75 mg or 11.25 mg with iron therapy is used before fibroid surgery to improve anemia due to vaginal bleeding from fibroids for patients in whom 3 months of hormonal suppression is deemed necessary. The duration of therapy with LUPRON DEPOT is limited to 3 months. The symptoms associated with fibroids will return after stopping therapy.
Your doctor may consider a 1-month trial of iron alone, as some women will respond to iron alone. Lupron Depot 3.75 mg or 11.25 mg may be added if the response to iron alone is considered inadequate.
Limitations of Use
Lupron Depot 3.75 mg or 11.25 mg is not used in combination with norethindrone acetate add-back therapy before fibroid surgery to improve anemia due to vaginal bleeding from fibroids.
If you have uterine fibroids, you are not alone…
An estimated 1 in 4 women with uterine fibroids suffers from symptoms that affect daily life.
What are Fibroids?
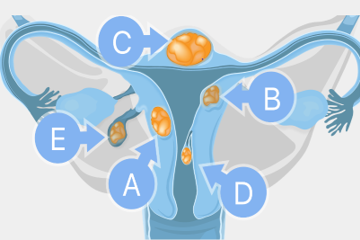
Uterine fibroids are growths (or tumors) that develop in the muscular wall of the uterus.
They may also be called myomas or leiomyomas uteri. Fibroids are generally benign—that is, they are not cancerous (malignant). Fibroids are the most common kind of growths of the uterus. A woman may have just one fibroid or several.
They may remain very small for a long time, then grow suddenly and rapidly—or they may grow slowly over a number of years.
Uterine fibroids can range in size from microscopic to the size of a grapefruit or even larger.
Types of Fibroids
Uterine fibroids can appear on different locations on the uterus:
a) Inside the uterus wall (intramural)
b) On the inner surface (submucosal)
c) On the outer surface (subserosal)
d) Attached to the inside of the uterus by a stem-like structure (pedunculated submucosal)
e) Attached to the outside of the uterus by a stem-like structure (pedunculated subserosal)
Causes of Fibroids and who is at Risk
It is not clear what causes fibroids, but evidence suggests that their growth is related to estrogen and progesterone. Fibroids are most common in women aged 30-40 years, but they can occur at any age.
Fibroids occur about 3 times more often in African American women.
Possible Symptoms Associated with Fibroids
The location and size of fibroids can determine the type and severity of your signs or symptoms.
The following are some possible signs, symptoms and complications of uterine fibroids:
– Heavy or prolonged menstrual bleeding
– Bleeding between periods
– Anemia
– Enlarged uterus or abdomen
– Pelvic pain or pressure
Anemia Related to Fibroids
Excessive bleeding due to fibroids may lead to anemia, which can make you feel abnormally tired. Other symptoms may include pale skin, feeling weak, shortness of breath, and cold hands and feet. People are considered anemic when they have a lower than normal amount of red blood cells in their blood. To assess this, a routine blood test measures the hemoglobin and hematocrit levels. Hemoglobin is the iron-containing protein found in red blood cells that carries oxygen from the lungs to the rest of your body. Hematocrit is a measure of the proportion of red blood cells in a sample of blood.
Raising hemoglobin and hematocrit levels prior to surgery is a treatment consideration you should discuss with your doctor.
Clinical studies have shown that Lupron Depot, when used in combination with iron, may raise hemoglobin and hematocrit levels.
Treatment Considerations
The treatment your doctor recommends may depend on medical history, your symptoms, the number of fibroids you have, and their location in the body. Surgical considerations may include a myomectomy or hysterectomy.
How Lupron Depot Works
Lupron Depot belongs to a class of drugs called gonadotropin-releasing hormone agonists (GnRHa). It works by decreasing the amount of estrogen that your ovaries produce.
Common Side Effects
Most common related adverse reactions (>10%) in clinical trials were hot flashes/sweats, headache/migraine, decreased libido, depression/emotional lability, dizziness, nausea/vomiting, pain, vaginitis, and weight gain.
Dosage and Length of Therapy
Lupron Depot is given in combination with iron therapy as a single injection lasting 3 months or given monthly for up to 3 injections prior to surgery.
One 3-month 11.25 mg injection
Three 1-month 3.75 mg injections
Lupron Depot Injections for Colon Cancer
Lupron Depot® (leuprolide acetate for depot suspension) 7.5 mg for 1-month, 22.5 mg for 3-month, 30 mg for 4-month, and 45 mg for 6-month administration are prescribed for the treatment of advanced prostate cancer. Lupron Depot is a prescription medication that must be administered in your doctor’s office.
Prostate Cancer
The prostate is part of the male reproductive system and produces fluid that makes up a part of semen.
Prostate cancer occurs when abnormal cells within the prostate gland grow out of control.
Testosterone plays an integral role in the growth and management of prostate cancer.
There are several types of prostate cancer:
Local/Localized

Local prostate cancer is a group of cells that grows faster than normal within a man’s prostate gland, which sits just below the bladder. Of men who are diagnosed with prostate cancer, 70% are diagnosed with localized prostate cancer.
Locally Advanced/Regional

Locally advanced prostate cancer is when the cancer cells have grown through the outer rim of the prostate and into nearby tissue. Of men who are diagnosed with prostate cancer, 13% are diagnosed with regional prostate cancer.
Metastatic/Distant
Metastatic prostate cancer is when the prostate cancer spreads, or metastasizes, to the lymph nodes or other parts of the body. Of men who are diagnosed with prostate cancer, 8% are diagnosed with distant prostate cancer.
Recurrent

Recurrent prostate cancer is when prostate cancer comes back after it was treated. The cancer can come back in or near the prostate or in another part of the body.
Who is at Risk?
All men are at risk for prostate cancer, and about 1 in 8 men will develop prostate cancer in their lifetime. Of those developing prostate cancer, approximately 21% will be diagnosed with advanced prostate cancer.
Age is the most common risk factor, and the older you are, the greater the risk of developing prostate cancer.
Men aged 50 and over who are at average risk of prostate cancer and have a life expectancy of at least 10 years should:
– Receive information about the potential benefits and known limitations of testing for early prostate cancer detection
– Be given the opportunity to make an informed decision about testing
Black American men are nearly 2x more likely to be diagnosed with prostate cancer compared with White American men. The death rate from prostate cancer in Black American men is twice as high as in White American men. Black American men should be given information about prostate cancer screening so that they can have discussions with their doctors at an earlier age than other men (45 vs 50 years old)
Men with a family history of prostate cancer may be at higher risk, so it’s important to talk to your doctor about your family’s health history.
Testosterone
Testosterone is a key hormone in men and is part of the normal growth and function of the prostate gland. In men who have prostate cancer, testosterone can help certain prostate cancer cells multiply. As a result, as long as the body produces testosterone, prostate cancer is likely to continue to grow and possibly spread.
What is PSA?
PSA is the abbreviation for prostate-specific antigen, a protein made by the prostate gland. A PSA test measures the level of PSA in the bloodstream, and the results are used to help identify disorders of the prostate, including prostate cancer.
Suppressing Testosterone
Testosterone suppression using androgen deprivation therapy (ADT) is the “gold standard” treatment to manage advanced prostate cancer. Testing your testosterone level in addition to your PSA level can give your doctor a more complete picture of how your body is responding to treatment.
Advanced Prostate Cancer Treatment Options
You and your doctor will work together to decide on a treatment plan that works best for you by considering your age, the stage of your disease, any other medical conditions, and your doctor’s recommendation.
Treatment options can include:
– Surgery
– Radiation therapy
– Cryotherapy
– Robotic surgery
– Chemotherapy
– ADT
Hormone Therapy and When it’s Used:
ADT is a form of hormone therapy that seeks to reduce the level of male hormones (called androgens) in the body, which fuel prostate cancer cells to grow.
A doctor may prescribe hormone therapy for advanced prostate cancer:
– If the cancer has spread too far to be cured by surgery or radiation, or if you can’t have these treatments for some other reason
– If the cancer remains or comes back after treatment with surgery or radiation therapy
– Along with radiation therapy as the initial treatment if you are at higher risk of the cancer coming back after treatment
(based on a high Gleason score, high PSA level, and/or growth of the cancer outside the prostate)
– Before radiation, to try and make treatment more effective
Common Side Effects of Lupron Depot
The most common side effects of Lupron Depot include hot flashes/sweats; injection site reaction/pain; general pain; swelling; testicular shrinkage; difficulty urinating; fatigue/weakness; headache; and joint, gastrointestinal, and respiratory problems.
Lupron Depot Injections Central Precocious Puberty (CPP)
Lupron Depot-PED® (leuprolide acetate for depot suspension) is an injectable prescription gonadotropin-releasing hormone (GnRH) medicine used for the treatment of children with central precocious puberty (CPP). It is not known if Lupron Depot-PED is safe and effective in children under 2 years of age.
Central Precocious Puberty (CPP)
Puberty that starts too soon is called precocious puberty. The most common type is Central Precocious Puberty (CPP). Children with CPP that is left untreated will keep going through puberty and that can have lasting complications beyond childhood.
If you suspect your child has CPP, don’t wait–act now and notify your child’s pediatrician. They can refer you to a pediatric endocrinologist who can appropriately diagnose your child and determine the right treatment plan for them.
Common Signs of Puberty-Girls:
– Irritability and mood swings
– Breast bud development
– Menstrual periods, pubic hair, vaginal discharge
– Oily skin/acne
– Underarm hair and adult body odor
– Sudden growth spurt
CPP is when puberty starts sooner than it should. For girls, that’s before the age of 8, and for boys, before the age of 9.
Common Signs of Puberty-Boys:
– Irritability and mood swings
– Underarm hair and adult body odor
– Testicle and penis enlargement, erections and pubic hair
– Voice change, facial hair, oily skin/acne
– Sudden growth spurt
Lupron Depot-PED
A gonadotropin-releasing hormone, or GnRH, agonist. It works by
helping the pituitary gland ignore signals from the brain. This, in turn,
stops the release of sex hormones that cause puberty

96.4% of children achieved suppression of a reproductive hormone. Suppression means either pausing puberty with no changes or reversing the signs of puberty.
How is Lupron Depot-PED Administered?
Your child’s doctor should do tests to make sure your child has CPP before treating them with Lupron Depot-PED. Lupron Depot-PED is given as a single-dose injection into your child’s muscle each month or every 3 months by a doctor or trained nurse. Your child’s doctor will decide how often your child will receive the injection. Keep all scheduled visits to the doctor. If a scheduled dose is missed, your child may start having signs of puberty again. The doctor will do regular exams and blood tests to check for signs of puberty.
Side effects of Lupron Depot-PED
The most common side effects of Lupron Depot-PED received 1 time each month include:
– Injection site reactions such as pain, swelling, and abscess
– Weight gain
– Pain throughout body
– Headache
– Acne or red, itchy rash and white scales (seborrhea)
– Serious skin rash (erythema multiforme)
– Mood changes
– Swelling of vagina (vaginitis), vaginal bleeding, and vaginal discharge
The most common side effects of Lupron Depot-PED received every 3 months include:
– Injection site reactions such as pain and swelling
– Weight gain
– Headache
– Mood changes
Important Safety Information
During the first 2 to 4 weeks of treatment, Lupron Depot-PED can cause an increase in some hormones. During this time, you may notice more signs of puberty in your child, including vaginal bleeding. Call your child’s doctor if these signs continue after the second month of treatment with Lupron Depot-PED.
Some people taking gonadotropin-releasing hormone (GnRH) agonists like Lupron Depot-PED have had new or worsened mental (psychiatric) problems. Mental (psychiatric) problems may include emotional symptoms such as:
– Crying
– Irritability
– Restlessness (impatience)
– Anger
– Acting aggressive
