Bipolar Disorder Introduction
Bipolar disorder is characterized by both manic and depressive symptoms. Manic symptoms include having flights of ideas, being more talkative, less need for sleep and increased distractibility. Depressive symptoms include fatigue or loss of energy, weight loss or gain, feeling worthless and in severe cases suicidal ideation. Some severe cases of bipolar disorder may even have psychotic symptoms as well. Bipolar disorder is a form of mental illness that affects 1 to 2% of our population1. It is also a mental illness that has one of the highest comorbidity and mortality rates as well; hence it is something of great concern3. When one is diagnosed with the disorder, their mood changes over months. It is a common misconception that those with bipolar disorder have a mood change within seconds (for example, from being happy to angry or sad), however this is not the case.
Causes of Bipolar Disorder
The exact cause of the disorder is not known, but evidence is showing that it is due to chemical imbalances in the brain. There is an increase in the amyglada volume and a decrease in the cortical volume in the brains of individuals who are bipolar5. Moreover, there is a decrease in serotonin, dopamine and glutamate in the brain as well, which are similar to the changes seen in depression. The role of norepinephrine has conflicting evidence, and some studies show increased levels, whereas others are showing decreased levels5. Moreover, gamma-Aminobutyric acid (GABA) deficiencies and excessive glutamate activity in the brain may also lead to alterations in neurotransmitter levels, hence leading to bipolar disorder5. Other theories include alteration in calcium channels, changes in circadian rhythms, mitochondrial dysfunction and increased protein kinase C (PKC) activity in the brain5. It seems that genetics also play a role in the disorder as well since there is evidence showing family history for the disorder.
Diagnoses
Bipolar disorder is usually diagnosed in adolescences, however in rare cases some older adults may be diagnosed later in life due to being misdiagnosed with other similar conditions throughout their lives. There is no diagnostic test for bipolar disorder (for example, a CT scan of the head will not diagnose one with the disorder). It is an illness that requires clinical diagnosis from a psychiatrist. Some psychiatrists may ask a patient to complete a Mood Disorder Questionnaire (MDQ), which helps them determine if mania or hypomania is present. Moreover, a psychiatrist may ask to speak with a close family member or friend of yours in order to get a better understanding of your mood from someone close to you. A family history of psychiatric conditions is also taken into consideration when making the diagnosis. Your psychiatrists may also refer to something called the DSM-5, which is short for The Diagnostic and Statistical Manual of Mental Disorders. This is a manual that is used to aid healthcare professional in diagnosing and treating psychiatric illnesses. A psychiatrist will first determine if you have had a manic episode, a hypomanic episode, or if you are on a depressive state. The table below will summarize this.
Describing the Bipolar Episodes2
| Type of Episode | Features |
| Manic Episode | Mood: Abnormally and persistently elevated, expansive or irritable; must have concomitant increase in activity or energy; psychotic symptoms may occur
Duration: At least 1 week, present most of the day, causing significant distress/disability or requiring hospital admission Plus: If mood is elevated or expansive, 3 or more of the following features must be present. If mood is predominantly irritable, 4 or more are required.
|
| Hypomanic Episode | Mood: Same symptoms as for mania, but milder and not disabling; no psychotic symptoms
Duration: 4 days or longer and present most of the day |
| Depressive Episode | Mood: Depressed most of the day or markedly diminished interest or pleasure
Duration: At least 2 week, with significant change from previous functioning Plus: Four or more of the following:
|
Using the above episodes, the disorder is diagnosed into three main categories, these consist of bipolar 1 disorder, bipolar 2 disorder, and other, which consists of the disorder being associated with a medication or substance use, another medical condition or other specified or unspecified reasons. These categories are summarized in the table below
Classification of Bipolar Disorders2
| Disorder | Features |
| Bipolar 1 Disorder | Lifetime history of at least 1 clear-cut manic episode, with or without episodes of hypomania or depression |
| Bipolar 2 Disorder | History of hypomanic episode and major depressive episodes, with no history of a full manic episode |
| Substance/Medication-Induced Bipolar and Related Disorder | Most diagnostic criteria for bipolar disorder met, but there is evidence that this developed during or soon after substance intoxication/withdrawal or medication use/withdrawal; the offending substance must be judged as capable of inducing such symptoms |
| Bipolar and Related Disorder due to Another Medical Condition | Most diagnostic criteria for bipolar disorder met, but there is evidence that this is the direct pathophysiological consequence of another medical condition |
| Other Specified (or unspecified) Bipolar and Related Disorders | Most diagnostic criteria for bipolar disorder met, but not all, e.g., duration of episode shorter than required for diagnosis, or history of hypomanic episodes but no depressive episodes that meet diagnostic criteria |
| Cyclothymic Disorder | Recurrent episodes of hypomania and mild (sub-threshold) depressive symptoms |
Non-Pharmacological Treatment
Medications are the mainstay of treatment when it comes to treating bipolar disorder. However, it is important that patients and close family members and friends are aware of worsening symptoms. This will allow your healthcare providers to provide a more efficient and effective treatment adjustment. Some very severe cases of bipolar disorder will use electroconvulsive therapy (ECT), however this option is usually reserved for those who have failed several different medications.
Pharmacological Treatment
As listed above, medications are the mainstay of treatment. Depending on what phase of the disorder you are in, manic, hypomanic or depressive, your medication may be changed in order to better accommodate your symptoms. Treatment is usually lifelong; however, discontinuing medications may be a possibility for some patients in the future. If you are newly diagnosed with bipolar disorder, the medication used during your acute phase (when you were first diagnosed and treated) may be the medication that is used during your maintenance phase4. However, in other cases the medication may be changed to better accommodate your symptoms and how you are responding to the pharmacological treatment. Medications used to treat bipolar disorder are usually used for a minimum to two weeks before symptom improvement for mania can be assessed, whereas it may take two to four weeks minimum before depressive symptoms start to improve3. Something of importance is that your physician will discontinue your antidepressant if you are diagnosed with bipolar disorder. Do not be alarmed if this happens because you will be put on another medication to help with your depressive symptoms. The reason for discontinuing the antidepressant and using another medication to aid with depressive symptoms is to prevent the induction of a manic phase in patients.
The two most common class of medications used to treat bipolar disorder are mood stabilizers, and antipsychotic medications, specifically second-generation antipsychotics (SGA). The three common mood stabilizers are lithium, divalproex and lamotrigine. The most common SGAs are quetiapine, aripiprazole, risperidone. The following will go into first line pharmaceutical treatments for bipolar disorder, along with common side effects, and drug interactions that your physician and pharmacist may notify you about. There will be a brief mention of second and third line options, but these will not be completely discussed in this blog, but more information about them can be found on The Canadian Network for Mood and Anxiety Treatment (CANMAT) Guidelines4. As a disclaimer, the following tables were obtained from the compendium of therapeutics 20193.
Table 1: Pharmacologic Management of Acute Mania in Bipolar Disorder4
| Place in Therapy | Drugs | Comments |
| First-line | lithium | While high blood lithium level produce more response, it involves more risk. Consider moderate blood levels (0.8–1.0 mmol/L) and add other anti-manic agents if necessary. Because of overall value, consider lithium first, particularly in younger adults. |
| quetiapine | Rapid dose titration is generally safe, but monitor for hypotension. | |
| divalproex | Loading dose is an option (20 mg/kg); aim for blood levels high in therapeutic range (350–800 mcmol/L). | |
| asenapine | Sublingual tablet; important not to eat or drink for 10 min after administration. | |
| aripiprazole | Limited benefit for depressed phase, less desirable in someone with a history of frequent depressive relapses. | |
| paliperidone >6 mg | Available as extended-release tablet and long-acting IM injection. | |
| risperidone | Monitor regularly for orthostatic hypotension and extrapyramidal side effects, e.g., parkinsonism, akathisia. | |
| lithium or divalproex plus quetiapine | Allows lower dosing of quetiapine than in monotherapy; useful for more severe episodes; start quetiapine first × 1–3 days. | |
| lithium or divalproex plus aripiprazole | Better tolerated than most other combination treatments. | |
| lithium or divalproex plus risperidone | Often can taper risperidone after 6 months of euthymia. Allows lower dosing of risperidone than in monotherapy; useful for more severe episodes; start risperidone first × 1–3 days. | |
| lithium or divalproex plus asenapine | Relatively well tolerated. | |
| Second-line | Try several first-line treatments first before going to second-line treatments. | |
| olanzapine | Slightly more effective than other SGAs, but far more long-term side effects. | |
| carbamazepine (including extended-release) | Watch for hepatic induction, which lowers blood levels of many medications, including key SGAs and some antidepressants. | |
| lithium or divalproex plus olanzapine | Good for severe episodes, but highest side effect burden in the long term. | |
| lithium plus divalproex | Less beneficial than combinations of a mood stabilizer plus SGA. | |
| ziprasidone | Limited evidence in maintenance, not effective for depression, cardiac monitoring at higher doses. | |
| haloperidol | Well tolerated and highly efficacious acutely, but promotes depression relapse and tardive dyskinesia concerns in the long term. | |
| ECT | Appropriate and effective for severe mania, and in medically ill. | |
Table 2: Pharmacologic Management of Acute Depression in Bipolar Disorder4
| Place in Therapy | Drugs | Comments |
| First-line | quetiapine (including extended-release) | Monotherapy studies showed doses of 300 or 600 mg/day to be equally effective; lower dose preferred if patient is medication-naïve. |
| lithium or divalproex plus lurasidone | Lurasidone must be taken with food—at least 350 calories.
Initiate lurasidone at 20 mg/day; titrate to lowest effective dose to minimize adverse effects. |
|
| lithium | Aim for blood levels near the high end of therapeutic range as tolerated, i.e., 1–1.2 mmol/L (0.5–0.8 mmol/L in elderly patients). Measure serum concentration 9–13 h post-dose.
May be useful for those with high risk of suicide or self harm. |
|
| lamotrigine | Slow titration schedule slows response but mitigates risk of adverse effects including rash; useful for milder episodes. | |
| lurasidone | Must be taken with food—at least 350 calories.
Initiate at 20 mg/day; titrate to lowest effective dose to minimize adverse effects. |
|
| adjunctive lamotrigine | Slow titration schedule slows response but mitigates risk of adverse effects including rash. | |
| Second-line | divalproex
adjunctive SSRI or bupropion ECT cariprazine olanzapine plus fluoxetine |
Try several first-line treatments before going to second-line options. |
| Third-line | Many choices exist (almost always as adjunctive treatments), including selected atypical antipsychotics, SNRI or MAOI antidepressants, IV ketamine, stimulants, light therapy, rTMS, and others | Third-line choices best initiated by mood disorder specialists. ECT may be initial treatment in particularly severe depression or in medically ill patients. |
Once a patient overcomes the acute phase of their illness, and they have been symptom free for at least two months, they are considered to be in remission. However, this does not mean the patient stops their medications. Some patients may be switched to a maintenance medication, whereas other may have a decrease in the dose of their medication that was used in the acute phase. The purpose of maintenance medication is because 70% of patients have a chance of experiencing another episode of mania or depression over the next year if they are left untreated3.
Table 3: Maintenance Treatment Regimens for Bipolar Disorder4
| Place in Therapy | Drugs | Comments | |
| First-line | lithium | Blood levels can be individualized—some patients have efficacy at lower end of normal therapeutic range (0.5–0.8 mmol/L); levels lower than for acute episode. Effective in preventing manic and depressive relapses. | |
| quetiapine | Effective in preventing both manic and depressive relapses. | ||
| divalproex | Moderate evidence supports effectiveness in both manic and depressive relapses. | ||
| lamotrigine | Effective primarily for prophylaxis against depressive relapses. | ||
| asenapine | Effective for both manic and depressive relapses. | ||
| lithium or divalproex plus quetiapine | Effective for both manic and depressive relapses. | ||
| lithium or divalproex plus aripiprazole | Effective primarily for prevention of manic relapse. | ||
| aripiprazole | Effective for prevention of manic relapse. | ||
| aripiprazole OM monotherapy | This depot injection is effective for prevention of manic relapse. | ||
| Second-line | Try several first-line treatments before going to second-line treatments. | ||
| olanzapine | Effective for preventing both manic and depressive relapses, but with high side effect burden. | ||
| risperidone LAI | Long-acting injection effective for preventing manic relapses. | ||
| adjunctive risperidone LAI | Long-acting injection effective for preventing manic relapses. | ||
| carbamazepine | Moderate evidence for prevention of both manic and depressive relapses, with significant side effect concerns. | ||
| paliperidone (>6 mg) | Primarily for prevention of manic relapse. | ||
| lithium or divalproex plus lurasidone | Limited evidence suggests effective for preventing depressive relapse, and very limited evidence suggests effective for preventing manic relapse. | ||
| lithium or divalproex plus ziprasidone | Primarily prevents manic relapse. | ||
| Third-line | aripiprazole plus lamotrigine
adjunctive clozapine adjunctive gabapentin olanzapine plus fluoxetine |
Third-line choices best reserved for mood disorder specialists. | |
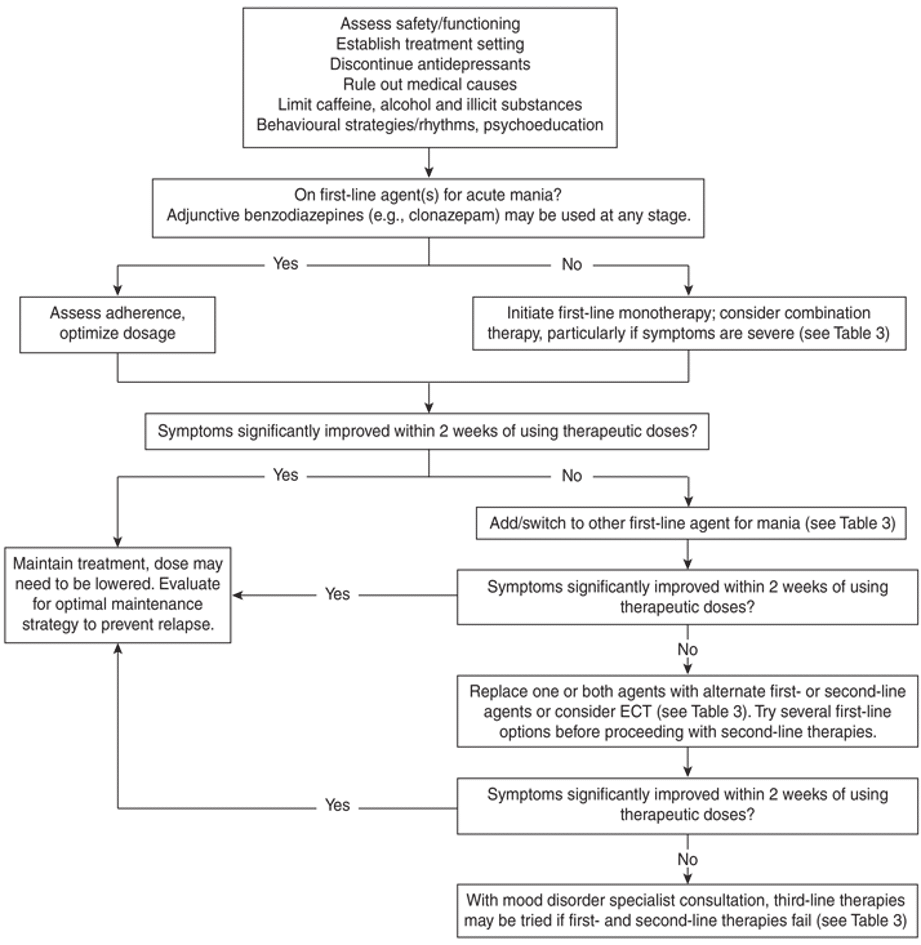
The following figure (figure 1) is a guideline to help healthcare processionals guide their choices and steps they take when helping you deal with ones acute mania phase of their bipolar disorder. It is important to note that this is just a guideline, and that your psychiatrists may choose another medication or approach when helping you deal with your disorder. Please refer to the compendium of therapeutics3 to see the algothrithm for depressive episodes and maintnence therapy.
Figure 1: Management of Acute Mania
Lithium
Mechanism of Action: The exact mechanism of action is not know, however lithium is a monovalent cation, and in the body it competes with other cations. Cations help with cellular functions such as releasing neurotransmitters. Lithium reduces excitatory neurotransmitters such as dopamine and glutamate and increases inhibitory neurotransmission, specifically GABA6. It has also shown to dampen the over activity of PKC in the brain as well6.
Side Effects: Some of the common side effects include: polyuria (excessive urination), polydipsia (excessive thirst), nausea, vomiting, fatigue, weight gain and tremor. Other less common ones are hair loss and hypothyroidism (low levels if the thyroid hormone)7.
Drug Interactions: Drugs that may increase the concentration of lithium and hence lead to lithium toxicity include ACE-Is, ARBs, Diuretics and NSAIDs7. Lithium toxicity is defined as having a serum level >1.5 mmol/L.
Usual Dose: The initial starting dose is 300 mg three times daily, to a usual maintenance dose of 900 – 2100 mg per day3. The dose of lithium is targeted to serum levels in the body. During acute mania or depression the serum levels are targeted between 0.8 to 1.2 mmol/L, but maintenance levels may range between 0.6 to 1.0 mmol/L. The levels are checked 13 hours post ingestion in the hospital. Once a patient is stabilized on a dose, levels are measured every three months unless another manic phase occurs, in which case they will be measured sooner.
| Manic Phase | Depressive Phase | Maintenance Phase |
| Initial: 300 mg TID PO (150 mg BID PO in the elderly)
Dose can be titrated up by increments of 300–600 mg/day every 5–7 days, depending on tolerability and response Usual: 900–2100 mg/day PO, guided by serum concentrations |
Initial: 300 mg TID PO (150 mg BID PO in the elderly)
Dose can be titrated up by increments of 300–600 mg/day every 5–7 days, depending on tolerability and response Usual: 600–1800 mg/day PO, guided by serum concentrations |
600–1800 mg/day PO, adjusted according to serum levels (target range 0.5–0.8 mmol/L |
Pregnancy and Lactation: Lithium does cross the placenta and enters breast milk. Talk to your healthcare provider if you become pregnant or are lactating while on lithium16.
Divalproex
Mechanism of Action: The exact mechanism of divalproex is not known, but it is suggested that it increases the GABA levels in the brain8. GABA has inhibitory effects in the brain, which results in a decrease in excitatory neurotransmitters such at glutamate.
Side Effects: Common side effects include nausea and vomiting, weight gain, dizziness, ataxia, and tremor. In rare cases, some patients may have a decrease in their platelets and white blood cells in the body. Hepatoxicity (liver damage) is also another severe, but rare side effect that could occur8.
Drug Interactions: Drugs that increase divalproex levels include, but are not limited to: ASA, cimetidine, erythromycin, fluoxetine and guanfacine. Drugs that decrease divalproex levels include, but are not limited to: carbamezapine, lamotrigine, phenobarbital, phenytoin, rifampin and meropenem, It is important to talk to your healthcare provider about what medications you take before initiating this medication3,8.
Usual Dose: The initial dose is 250 mg three times daily. The dose can be slowly titrated up by 250 to 500 mg every 3 days until at a target dose of 750 to 2000 mg a day3.
| Manic Phase | Depressive Phase | Maintenance Phase |
| Initial: 250 mg TID PO
Dose can be titrated up by increments of 250–500 mg/day every 1–3 days depending on tolerability Usual dose: 750–2000 mg/day PO |
Not first line | 750–2000 mg/day PO, adjusted according to serum levels |
Pregnancy and Lactation: Divalproex is contraindicated in pregnancy because it can cause birth defects, however it is a medication that is highly protein bound hence it can be used in females who are breast feeding because it is highly protein bound16.
Lamotrigine
Mechanism of Action: Lamotrigine acts on sodium voltage channels on neuronal membranes. This in turn results in less excitatory amino acids being released from neurons (examples include glutamate)9.
Side Effects: Stevens Johnson Syndrome is a severe reaction where a patient has flu like symptoms and breaks out in a red color all over their body with blisters. It is a reaction that could result in death9. Other more common side effects include dizziness, headache diplopia (double vision), somnolence, ataxia and nausea9.
Drug Interactions: Drugs that can increase lamotrigine levels, and hence increase the risk of side effects include divalproex, divalproex has shown to increase lamotrigine levels by almost 2 fold. Drugs that can decrease lamotrigine levels include, but are not limited to: carbamazepine, phenytoin, phenobarbital and primidone9.
Usual Dose: The usual initial dose is 25 mg daily, which is then slowly increased by 25 to 50 mg weekly to a usual target dose of 150 to 250 mg twice a day. If a patient has missed more than 5 consecutive days of their dose, it is suggested that they are titrated up from 25 mg again.
| Manic Phase | Depressive Phase | Maintenance Phase |
| Not first line | Initial: 25 mg once daily PO
Increase to 25 mg BID PO after 2 wk, then by 25–50 mg/day increments every 1–2 wk Usual dose: 100–300 mg/day PO |
100–300 mg/day PO |
Pregnancy and Lactation: Lamotrigine should only be used during pregnancy if the benefits outweigh the risks. Some post-marking studies have shown that there is a slight increased risk of oral cleft malformations when used during the first trimester, however the large sum of data shows that it is safe in pregnancy. Lactating females should avoid lamotrigine because it is excreted into breast milk, and the levels reaching the infant are similar to those in the mother16.
Quetiapine
Mechanism of Action: Quetiapine is a SGA. It works in the body by working as an antagonist at D2 dopamine receptors and serotonergic receptors, specifically the 5-HT2A receptor3,10.
Side Effects: The common side effects include somnolence, dizziness, dry mouth, elevation of serum triglycerides (increased LDL, decreased HDL), QTc prolongation, weight gain and in severe cases extrapyramidal symptoms, which are spams and motor restlessness in the body10.
Drug Interactions: Quetiapine is a medication that is known to cause QTc prolongation. It should be advised that co-administration with other medications that are known to cause QTc prolongation should be avoided10. Also, the rapid dose increases that happen with newly diagnosed bipolar disorder cases could cause some hypotension in patients, hence this is something to monitor for10.
Usual Dose:
| Manic Phase | Depressive Phase | Maintenance Phase |
| Day 1: 50 mg BID PO
Day 2: 100 mg BID PO Day 3: 150 mg BID PO Day 4: 200 mg BID PO Day 5 (if necessary): 300 mg BID PO Day 6 (if necessary): 400 mg BID PO Usual dose: 200–400 mg BID |
Day 1: 50 mg/day PO
Day 2: 100 mg/day PO Day 3: 200 mg/day PO Day 4: 300 mg/day PO Usual dose: 300 mg/day PO Maximum: 600 mg/day PO |
Usual: 300 mg/day PO
Maximum: 600 mg/day |
Pregnancy and Lactation: Quetiapine is safe to use during pregnancy because of the potential benefit to the mother is greater than the risk to the fetus. However, there is a potential toxicity to the infant when mothers are breastfeeding, hence precaution is required16.
Asenapine
Mechanism of Action: Asenapine is a SGA. It works in the body by working as an antagonist at D2 dopamine receptors and serotonergic receptors, specifically the 5-HT2A receptor11.
Side Effects: Some common side effects include weight gain, increased appetite, dizziness, sleepiness, fatigue, slow movements and tremor and involuntary muscle contractions11.
Drug Interactions: Asenapine is a newer medication, hence all the data on drug interactions is not completely known yet. One study showed that the co-administration of asenapine along with fluvoxamine resulted in higher levels of asenapine in the body11. Because of this, if you are also taking any SSRIs or SNRIs, let your physician or pharmacist know.
Usual Dose: Asenapine is the only medication used to treat bipolar disorder than is sublingual. The initial dose is 5 mg SL BID and can be increased to 10 mg SL BID.
| Manic Phase | Depressive Phase | Maintenance Phase |
| Initial: 5 mg BID SL
Dose can be slowly increased to a maximum of 10 mg BID SL depending on response and tolerability |
Not recommended | 5 mg BID SL
Maximum: 10 mg BID SL |
SL = Sublingual
Pregnancy and Lactation: There is no human data on the use of Asenapine during pregnancy or lactation, hence it should be avoided16
Lurasidone
Mechanism of Action: Lurasidone is a SGA. It works in the body by working as an antagonist at D2 dopamine receptors and serotonergic receptors, specifically the 5-HT2A receptor12.
Side effects: The common side effects include nausea, somnolence, akathisia (agitation and restlessness), and parkinsonism (movement disorders similar to Parkinson Disease, tremor, moving slowly etc…)3,12.
Drug Interactions: Lurasidone is broken down by CYP3A4. Medications that are inhibitors of CYP3A4, such as ketoconazole and diltiazem should be avoided because they will result in higher levels of lurasidone. On the other hand, medications that are inducers of CYP3A4, such as rifampin will result in lower levels of lurasidone in the body12.
Usual Dose: Lurasidone is a medication that should be taken with a minimum of 350-calorie meal.
| Manic Phase | Depressive Phase | Maintenance Phase |
| Not recommended | Initial: 20 mg/day PO with food (at least 350 calories)
Usual range: 20–60 mg/day Maximum: 120 mg/day |
Usual range: 20–60 mg/day
Maximum: 120 mg/day |
Pregnancy and Lactation: There is no human data on the use of lurasidone during pregnancy. Some research shows that the potential toxicity is only during the third trimester, but since it lacks human data, it should be avoided. Lurasidone should be avoided in lactation because there is no human data16.
Risperidone
Mechanism of Action: Risperidone is a SGA. It works in the body by working as an antagonist at D2 dopamine receptors and serotonergic receptors, specifically the 5-HT2A receptor13.
Side Effects: Common side effects include sedation, drowsiness, fatigue, weight gain, increased appetite, extrapyramidal symptoms and orthostasis (when the body rocks back and forth when standing upright)13.
Drug Interactions: Risperidone is broken down by CYP3A4 and 2D6 in the body. Inhibitors or inducers of these enzymes may effect the risperidone levels. Some common drugs that may increase risperidone in the body are fluoxetine, paroxetine, erythromycin, ketoconazole and verapamil. One thing to note is that risperidone oral tablets are not combatable with tea and cola, hence do not take the two together. It is also a drug that increases QTc prolongation, hence monitor when taking with other medications that are known to prolong QTc3, 13.
Usual Dose: Risperidone is one of the antipsychotic medications that can be given by the IM route
| Manic Phase | Depressive Phase | Maintenance Phase |
| Initial: 2–3 mg/day PO
Dose can be titrated up by increments of 1 mg/day every 24 h Usual dose: 3–6 mg/day in a single daily dose or 2 divided doses Risperidone IM injection Initial 25 mg IM every 2 weeks, increase my 12.5 mg every 4 weeks until a maximum of 50 mg IM every 2 weeks is reached. |
Not recommended | Not recommended |
Pregnancy and Lactation: When used in the third trimester, there has been evidence showing withdrawal symptoms in the newborns, however the benefits to the mother outweigh the risks to the infant, hence it is combatable with pregnancy16. There is limited human data when it comes to breast-feeding infants. Risperidone does cross into breast milk in low amounts, but there were no abnormalities in these breastfed infants. Since human data is lacking, there is still a risk for potential toxicity in lactating females16.
Paliperidone
Mechanism of Action: Paliperidone is a SGA. It works in the body by working as an antagonist at D2 dopamine receptors and serotonergic receptors, specifically the 5-HT2A receptor14.
Side Effects: Some of the common side effects include insomnia, headaches, weight gain, orthostasis, fatigue and extrapyramidal symptoms3.
Drug Interactions: Paliperidone is safe with many medications because it has minimum effect on the CYP enzymes. One common interaction to monitor for is the co-administration with carbamazepine, which results in decreased concentrations of paliperidone3,14.
Usual Dose: Paliperidone is available both as an oral tablet and a IM injection
| Manic Phase | Depressive Phase | Maintenance Phase |
| Initial: 3–6 mg/day PO
Dose can be titrated up by increments of 3 mg/day every 3–5 days Maximum: 12 mg/day Paliperidone IM injection 150 mg IM day 1 then 100 mg IM day 8 followed by maintenance doses between 50 to 150 mg IM every 4 weeks |
Not recommended | Not recommended |
Paliperidone oral tablets can also be switched over to the IM via the following
Table 4: Switching oral paliperidone to IM injection14
| Formulation | INVEGA Extended-Release Tablets | INVEGA SUSTENNA Prolonged-Release Injectable Suspension |
| Dosing Frequency | Once Daily | Once every 4 weeks |
| Dose (mg) | 12 | 150 |
| 6 | 75 | |
| 3 | 25–50 |
Note: this table was obtained from the Invega monograph via CPS
Pregnancy and Lactation: There is no data on the risk of paliperidone in pregnancy, but when looking as risperidone, which is a similar drug the evidence shows withdrawal symptoms in the newborns, however the benefits to the mother outweigh the risks to the infant, hence combatable with pregnancy16. Also the animal data shows low risk when used during pregnancy. There is limited human data with the use of paliperidone and breast-feeding, hence it should be avoided because of a potential toxicity to the infant16.
Aripiprazole
Mechanism of Action: Aripiprazole is a third generation antipsychotic. It works similarly to the SGAs by having antagonist effects of D2 and 5-HT2A receptors, however it also has a partial agonist effect on the dopamine receptors as well. This results in less extrapyramidal symptoms, which are movements disorders experienced by people who are on psychiatric medications15.
Side Effects: Common side effects include akathisia (a state where one is restless), dizziness, orthostatic hypotension (when one gets lightheaded while standing up), headaches, tremor and sedation. A less common side effect with aripiprazole is extrapyramidal symptoms3, 15.
Drug Interactions: Aripiprazole is broken down by CYP 3A4 and 2D6. Some drugs that may decrease levels of aripiprazole in the body are carbamazepine, phenytoin and rifampin. Drugs that may increase levels of aripiprazole in the body are fluoxetine, paroxetine and ketoconazole3, 15.
Usual Dose: Aripiprazole is also another treatment option that can be delivered via IM injection
| Manic Phase | Depressive Phase | Maintenance Phase |
| Initial: 15 mg/day PO in monotherapy or 10–15 mg/day PO if combined with lithium or divalproex
Dose can be increased after 2 week Maximum: 30 mg/day |
Not recommended | 15 mg/day PO
Maximum: 30 mg/day OR 400 mg once monthly by deep IM injection |
Pregnancy and Lactation: Human data has shown that there is a low risk of using aripiprazole during pregnancy, and that there is a low risk of developmental toxicity16. Aripiprazole does concentrate in breast milk, but very low amounts of it. With this said, there is still potential toxicity hence it should be avoided. One thing to note is that the use of aripiprazole in breastfeeding women resulted in lower lactation16.
Conclusion
It is important to note that bipolar disorder is a very complex and difficult disorder to treat. Your healthcare team may use medications that were listed here, or others that were not mentioned. Moreover, they may use the medications listed here, but at doses that were not mentioned here. Each individual is different, and their individual needs will also differ when it comes to their pharmaceutical treatment when treating bipolar disorder, hence the reason for some difference that you may notice. In addition, before treating your bipolar disorder, your healthcare team may start off by treating a substance dependence problems or another medical condition that is associated with your bipolar disorder. Treatment for most individuals is life long because the risk of a relapse is very high, especially in those who had a manic episode.
References
- Yatham, L.N., Kennedy, S.H., O’Donovan, C., Parikh, S., MacQueen, G., McIntyre, R., Sharma, V., Silverstone, P., Alda, M., Baruch, P., Beaulieu, S., Daigneault, A., Milev, R., Young, L.T., Ravindran, A., Schaffer, A., Connolly, M. and Gorman, C.P. (2005), Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines for the management of patients with bipolar disorder: consensus and controversies. Bipolar Disorders, 7: 5-69. doi:10.1111/j.1399-5618.2005.00219.x
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5thed. Washington (DC): American Psychiatric Publishing; 2013
- Parikh V. Sagar In CTC [Internet]. Ottawa (ON) Bipolar Disorder. Compendium of Therapeutics 2019 [cited 2020 January 8].
- Yatham, LN, Kennedy, SH, Parikh, SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018; 20: 97– 170. https://doi-org.ezproxy.library.ubc.ca/10.1111/bdi.12609
- Manji K. Husseini et al. (2003). The underlying neurobiology of bipolar disorder. World Psychiatry. 2(3). Pg. 136 – 146.
- Malhi, G.S., Tanious, M., Das, P. et al.Potential Mechanisms of Action of Lithium in Bipolar Disorder.CNS Drugs27, 135–153 (2013) doi:10.1007/s40263-013-0039-0
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Lithium. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Apo-Valproic Capsules. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Lamotrigine. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Seroquel. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Saphrix. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Latuda. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Risperdal. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Invega. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- CPS [Internet]. Ottawa, ON: Canadian Pharmacists Association; 2019 [cited 2020 Jan 10]. Abilify. Available from: http://www.e-therapeutics.ca. Also available in paper copy from the publisher.
- Briggs G.G., Freeman R.K., & Yaffe S. J. (2015). Drugs in pregnancy and lactation: a reference guide to fetal and neonatal risk. Tenth Edition. Philadelphia: Wolters/Kulwer/Lippinicott Williams & Wilkins Health.